- What is Classified as a Traumatic Event?
- Common Experiences Immediately After a Traumatic Event
- What Are The Symptoms of Post-Traumatic Stress Disorder (PTSD)?
- Complex Post-Traumatic Stress Disorder (CPTSD)
- Are Some People More at Risk of Developing Post-Traumatic Stress Disorder (PTSD)?
- Therapy Recommended For Post-Traumatic Stress Disorder (PTSD)
- Psychological Therapy Treatment for Post-Traumatic Stress Disorder (PTSD)
- Trauma-Focused Cognitive Behavioural Therapy (CBT)
- Trauma Therapy Near Me
- Eye movement desensitisation reprocessing (EMDR)
- EMDR Therapy Near Me
- Post-Traumatic Stress Disorder (PTSD) treatment over Telehealth
- What to do if I Think I Might Have Post-Traumatic Stress Disorder (PTSD)
- Lifestyle – mindfulness, exercise and self-help.
Post-Traumatic Stress Disorder (PTSD)
Post-traumatic stress disorder is a mental health condition that a person can develop after experiencing a traumatic event. PTSD is induced by trauma. If left untreated, PTSD can have a severe impact on a person’s daily life. Not everyone who experiences a traumatic event will develop post-traumatic stress disorder. An estimated 11% of Australians will experience PTSD in their lifetime.
PTSD can often co-occur with other mental health conditions including depression, anxiety disorders, substance use disorders and physical health issues such as chronic pain. Effective treatment involves addressing both the post traumatic stress disorder and these co-occurring conditions simultaneously.
What is Classified as a Traumatic Event?
A traumatic event is an event that threatens the life or physical safety of a person or that of their loved ones. The threat can be actual or perceived and can be experienced either in a single instance or repeatedly over a period of time.
Traumatic events can include:
War
Terrorism
Physical assault
Natural disasters
Accidents (bus, car, plane etc)
Torture
Sexual assault
A traumatic event can be experienced directly (physically experienced or witnessed) or indirectly (learnt about) (Pheonix Australia)
Common Experiences Immediately After a Traumatic Event
Immediately after a traumatic event it’s normal to experience distress and feel upset when reminded of the event. While we can all respond differently, it can be common to experience things like loss of memory and changes in the way we act. It can also be common to avoid certain feelings and situations.
It can take days to a few months to recover from a traumatic event. Gradually, with the help of our family, friends and other support networks, the feelings of distress generally reduce with time.
For some people, these feelings don’t get better with time and can instead have ongoing disruption to their everyday life. If feelings continue for a month after the event, it can be a sign of PTSD (RCPsych).
What Are The Symptoms of Post-Traumatic Stress Disorder (PTSD)?
The symptoms of PTSD can fall into four main groups
Avoidance
This is when a person avoids engaging in activities, going places or seeing people who can trigger memories of a traumatic event.
Negative alterations in cognition and mood
Including an inability to feel positive emotions coupled with persistent negative cognitions and emotions such as fear and guilt. A person may also experience unhelpful distorted thinking such as self-blame.
Hyper-arousal
Hyper-arousal can present as being constantly alert to signs of danger. Finding it hard to fall and stay asleep. Irritability, anger, poor concentration and memory.
Re-experiencing or intrusive symptoms
This can include unwanted thoughts, flashbacks and nightmares. When re-experiencing people can feel distressed and other physical responses like sweating and increased heart rate. (Pheonix Australia)
Complex Post-Traumatic Stress Disorder (CPTSD)
A person can develop complex post traumatic stress disorder (CPTSD) as a result of exposure to chronic trauma. Complex PTSD has many of the same symptoms as PTSD however generally with additional symptoms:
1. Difficulties with emotions
2. Difficulties with relationships
3. Negative self view

Are Some People More at Risk of Developing Post-Traumatic Stress Disorder (PTSD)?
Not everyone who experiences a traumatic event will develop post-traumatic stress disorder. Some of the things that may increase the chance of someone developing PTSD include:
1. Experiencing previous trauma
2. Experiencing homelessness
3. Having a personal or family history of mental illness or substance abuse
4. Lacking a network of family, friends and community to provide support after the event
5. Having additional unrelated life challenges such as job loss or death of a family member, coincide with the timing of the traumatic event
Some occupations are also at greater risk of developing post traumatic stress disorder. This includes members of emergency services, armed forces and veterans.
Therapy Recommended For Post-Traumatic Stress Disorder (PTSD)
In Australia the treatment options for PTSD fall into three main groups.
1. Physical treatments – For example medications. Not everyone with PTSD will need medication. You will need to speak with you doctor about medications.
2. Lifestyle – mindfulness, exercise and self-help.
3. Psychological therapy.
Treatment for PTSD can involve a combination of these three groups
Psychological Therapy Treatment for Post-Traumatic Stress Disorder (PTSD)
The recommended psychological therapies for PTSD in Australia are trauma-focused cognitive behavioural therapy (CBT) and eye movement desensitisation reprocessing (EMDR) (Martin et al, 2021).
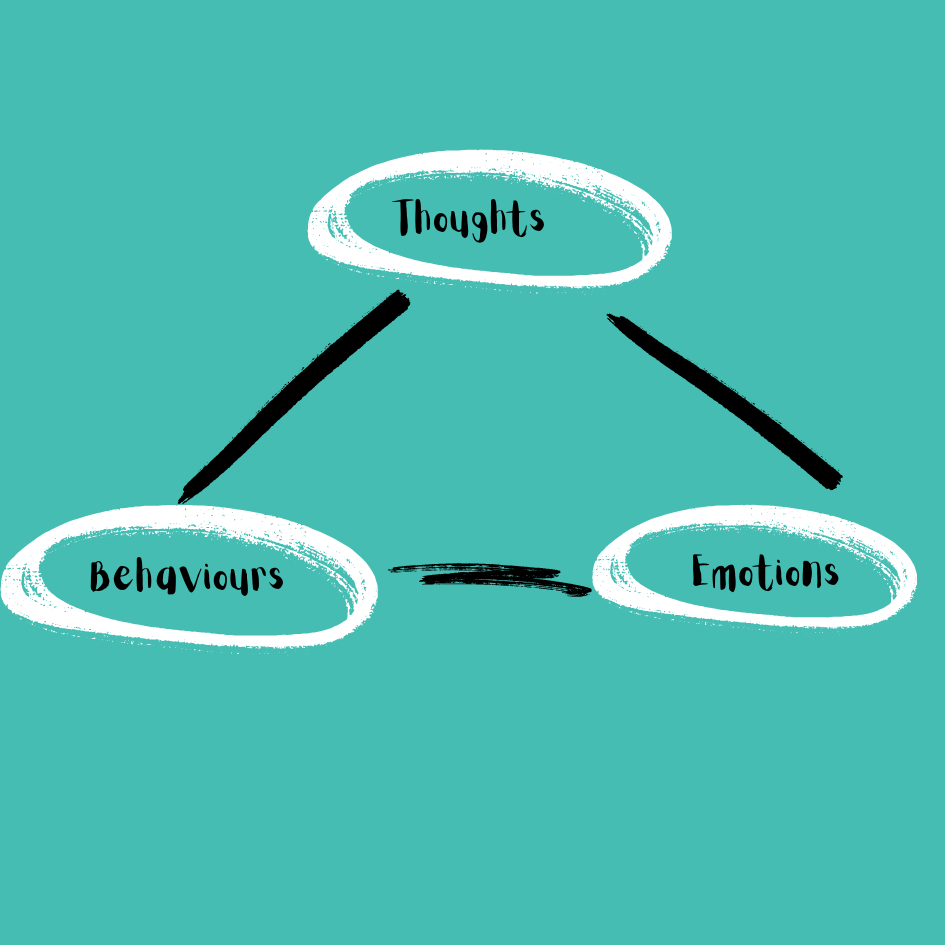
Trauma-Focused Cognitive Behavioural Therapy (CBT)
Trauma focused cognitive behaviour therapy was developed to treat individuals who have experienced trauma. It integrates trauma-sensitive interventions with CBT principles to address the emotional and psychological effects of traumatic experiences. Cognitive behaviour therapy is a talking therapy that explores the connection between our thoughts, emotions and behaviours. Key elements of Trauma-focused cognitive behavioural therapy include:
Psychoeducation –This is education about the common reactions to trauma exposure. Understanding these reactions can help normalise your experience and help reduce any feelings of isolation
Coping skills – including relaxation skills such as deep breathing, progressive muscle relaxation and mindfulness. Cognitive processing skills can also assist with challenging negative thoughts.
Gradual exposure – for example through imagining or by gradual exposure in real life in between sessions. Your psychologist will show you how to manage your anxiety and cope in this feared situation.
Cognitive processing of trauma related thoughts and beliefs – This can involve identifying and challenging unhelpful ways of thinking that have developed as a result of the trauma and replacing with more helpful thinking patterns (Arellano et al 2014).
Trauma Therapy Near Me
Meet Jayney Sutcliffe

Trained in CBT and trauma focused therapy, Jayneys special interests are Anxiety Disorders, Trauma, Depression and Domestic Violence. Taking a relaxed approach, Jayney makes every effort to offer clients a safe space where they feel secure enough to share their life experiences. Jayney says “I will offer you empathy and you will no longer feel so alone. You will walk away each time with skills to practice in better managing your struggles. I remind my clients Life always needs practice and rehearsal. I will be your coach.”
You can schedule a session with Jayney by submitting an enquiry
Eye movement desensitisation reprocessing (EMDR)
Eye movement desensitisation reprocessing (EMDR) is an accelerated information processing technique. The theory behind EMDR is that trauma can overwhelm the brain’s natural ability to process experiences, resulting in events being stored maladaptively and becoming “blocked”. EMDR helps by unlocking these memories and allowing the brain to integrate them properly, which can lead to decreased distress and improved mental health.
During an EMDR session, the therapist will ask their client to recall the traumatic memory that is still having an effect on them and via bilateral stimulation such as moving their eyes back and forth, help them to process the memory. By helping the brain reprocess the traumatic memory, it can help to reduce its emotional impact (Klockner, 2018).
EMDR Therapy Near Me
Meet Thomas Tran

You can schedule a session with Thomas by submitting an enquiry
Thomas is passionate about working from a person-centred approach as he incorporates various evidence-based treatment modalities into his practice to support clients towards achieving their therapeutic goals. These include Cognitive Behaviour Therapy (CBT), Acceptance and Commitment Therapy (ACT), Motivational Interviewing, Eye Movement Desensitisation and Reprocessing (EMDR), and Solution Focused Therapy.
Thomas provides therapy in both English and Vietnamese
Post-Traumatic Stress Disorder (PTSD) treatment over Telehealth
During the pandemic in particular, studies demonstrated that trauma focused cognitive behaviour therapy could be delivered just as effectively via telehealth and via the same treatments components as are applied in face to face (wild et al 2020).

What to do if I Think I Might Have Post-Traumatic Stress Disorder (PTSD)
Seeking help is the first step in treatment for PTSD and it’s important to seek help early. You can make an appointment to see your GP, psychologist or other mental health professional. You don’t need a referral from your GP to see a psychologist, however your GP may be able to create a Mental Health Treatment Plan (also known as a Mental Health Care Plan) for you.
What is a Mental Health Treatment Plan?
If your doctor diagnoses you with a mental health condition, they can create a plan with you to treat it. This plan is called a mental health treatment plan. As part of the plan, you will outline your goals and your treatment options and your doctor may refer you to a psychologist. Once completed, the plan will provide you access to up to 10 Medicare rebateable individual mental health services per calendar year. A rebate of $96.65 can be claimed on psychology sessions accessed with a mental health treatment plan. To access the rebate, you will need to provide your psychologist a copy of your mental health treatment plan and your GP referral
Some of the conditions that are eligible for a mental health treatment plan include:
Anxiety related conditions – panic disorder, obsessive compulsive disorder, post traumatic stress disorder, generalised anxiety disorder and phobias
Bipolar disorder
Depression
If you are seeking help with PTSD the experienced psychologists at Jelly Health are ready to support you. To schedule a session you can call 1300 281 540 or submit a request here.
Jelly Health is not an emergency service. If you are experiencing severe distress requiring an urgent response, call 000 or Lifeline on 13 11 14.
Lifestyle – mindfulness, exercise and self-help.
In addition to seeking therapeutic support, it’s also important that we look after our wellbeing. Here are some self-care tips.
- Eat nutritious meals – doesn’t need to be fancy, just good nourishing food
- Prioritise sleep
- Get some exercise – taking the dog for a walk is fantastic
- Spend some time doing an activity that you enjoy
- Keep connected with your community
- Spend time in nature and get some sunshine
References
De Arellano MA, Lyman DR, Jobe-Shields L, George P, Dougherty RH, Daniels AS, Ghose SS, Huang L, Delphin-Rittmon ME. Trauma-focused cognitive-behavioral therapy for children and adolescents: assessing the evidence. Psychiatr Serv. 2014 May 1;65(5):591-602. doi: 10.1176/appi.ps.201300255. PMID: 24638076; PMCID: PMC4396183.
https://www.rcpsych.ac.uk/mental-health/mental-illnesses-and-mental-health-problems/coping-after-a-traumatic-event
Dr Karen Klockner Department of Transport, Emergency and Safety Sciences School of Medical, Health and Allied Services Central Queensland University Brisbane, Australia (Paper Presented at the Australian and New Zealand Disaster and Emergency Management Conference Broadbeach, Gold Coast (QLD), 21 – 23 May 2018)
Martin A, Naunton M, Kosari S, Peterson G, Thomas J, Christenson JK. Treatment Guidelines for PTSD: A Systematic Review. Journal of Clinical Medicine. 2021; 10(18):4175. https://doi.org/10.3390/jcm10184175
Pheonix Australia, Australian PTSD Guidelines
Royal College of Psychiatrists, Coping After a Traumatic Event
Wild, J., Warnock-Parkes, E., Murray, H., Kerr, A., Thew, G., Grey, N., … Ehlers, A. (2020). Treating posttraumatic stress disorder remotely with cognitive therapy for PTSD. European Journal of Psychotraumatology, 11(1). https://doi.org/10.1080/20008198.2020.1785818