Cognitive Behaviour Therapy Near Me
Cognitive behaviour therapy (CBT) is one of the evidence based treatment modalities used by the psychologists at Jelly Health. All of the psychologists at Jelly Health are experienced CBT professionals. At Jelly Health you can access therapy online Australia wide. This blog provides a general overview of cognitive behaviour therapy, why it’s popular and things to be prepared for when starting therapy.
Cognitive Behaviour Therapy
Cognitive behaviour therapy is one of the most well know and widely used forms of talk therapy in the world. CBT was developed by Dr. Aaron T. Beck in the 1960s, initially focusing on depression but later expanding to other mental health issues (Beck, 2021). Today cognitive behaviour therapy is one of the most extensively researched of all psychotherapies, with several evidence based treatment protocols. There is a strong evidence base that CBT can improve the lives of people living with a range of mental and physical conditions (Fordham et al, 2021).
How Does Cognitive Behaviour Therapy (CBT) Work?
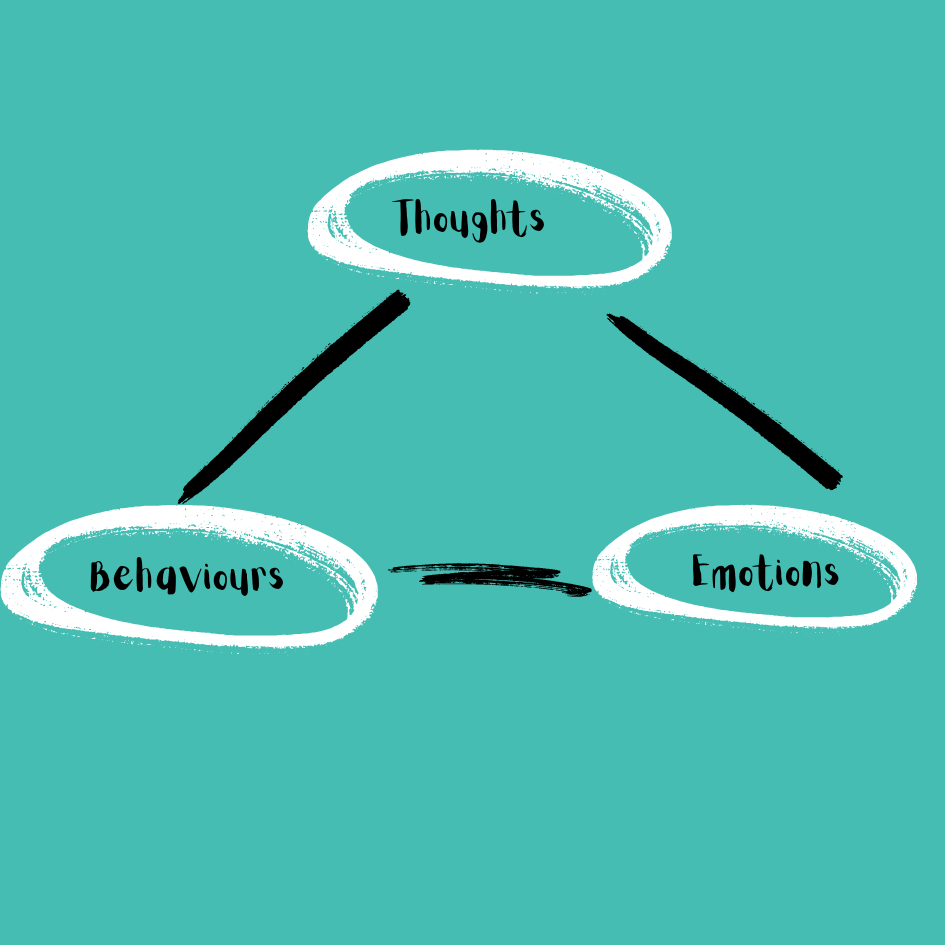
As the name suggests, cognitive behaviour therapy focuses on our thoughts and our behaviours. More specifically it explores the connections between our thoughts, emotions and behaviours. The basis of cognitive behaviour therapy is the theory that it is how we perceive or think about a situation that determines how we react to it. Not the situation itself (Fenn et al 2013).
Cognitive behaviour therapy describes the three aspects of cognition (Chand et al)
1. Automatic thoughts
2. Cognitive distortions
3. Underlying beliefs
Automatic Thoughts
These are the involuntary thoughts that come immediately to us as we interpret events happening around us. We are not always conscious of our automatic thoughts and may require some effort to recognise them. Our automatic thoughts can impact our emotions and behaviours. For example, imagine a situation where you are walking down the street and see a friend. The friend does not say hello to you. One automatic thought could be “I must have done something to upset them,” which may lead to feelings of anxiety or guilt. Conversely a different automatic thought could be “they must be in a hurry,” which can lead to more neutral feelings and understanding. (Chand et al)
Cognitive Distortions
Distorted ways in thinking can lead us to make erroneous decisions. These patterns of thinking can sometimes be learned. CBT helps us to identify and change these patterns of thinking. Examples of cognitive distortions (unhelpful ways of thinking) include:
• All or nothing (black and white) thinking: I need to get an A or I have failed.
• Jumping to conclusions: I can’t answer the first question, I’m going to fail the test.
• Generalising: Reaching a universal conclusion based on one event. Eg – I’ll never be happy
• Mind reading: Jumping to conclusion about what another person is thinking.
• Comparison: All my friends are happier than me
• Catastrophising: I missed a promotion; my career is ruined. I’ll never be successful
• Labelling: I’m not that smart a person
• Disqualifying the positive: I only got selected because there was no one else to choose
• Blaming: Blaming either others or holding yourself overly responsible for anything bad that happens
• Filtering and magnifying: When we only pay attention to and exaggerate the importance of information that fits with our beliefs and assumptions.
(Briers, 2014)
Emotional Reasoning
Emotional reasoning is another unhelpful way of thinking where we interpret situation based solely on our emotions. In short, I feel therefore it is. For example, if you were feeling anxious, you would conclude that something bad was going to happen based solely on your anxious feeling without looking at all the facts of a situation.
Beliefs and Assumptions
While we may not be aware of it, we all have our own beliefs and assumptions that shape the way that we see the world. We all see and interpret the world through our own lense. Our beliefs develop as we go through life and sometimes these beliefs and assumptions can result in unhelpful thoughts and behaviours. An example of an unhelpful belief is “The world is a dangerous place”
During cognitive behaviour therapy we get to understand our current ways of thinking and behaving and learn tools to help us adapt unhelpful thinking and behaviour patterns. Depending on the reason for seeking therapy, cognitive behaviour therapy can consist of the application of number of different techniques. Your psychologist will tailor your therapy specifically for you. Below are some examples of strategies. Not all CBT will use all these strategies (APA, 2017).
Strategies to change thinking patterns:
• Learning to recognise our own cognitive distortions or unhelpful ways of thinking. Learning how to challenge these cognitive distortions and replace them with more helpful ways of thinking.
• Learning how to use problem solving skills to deal with challenging situations.
• Gaining insight and a better understanding of the motivation and behaviour of others
• Developing confidence in our own abilities
Strategies to change behaviour patterns:
• Learning relaxation techniques
• Using role playing for potentially problematic interactions
• Exposure. Learning to do some on the things we avoid
Cognitive Behaviour Therapy is a Popular Therapy
There are a number of reasons why cognitive behaviour therapy is such a widely used therapy.
It can be easy to understand
The basic concepts of cognitive behaviour therapy around thoughts, behaviours and emotions are relatively easy for people to understand. This makes it more accessible and appealing. Some call it the psychology of common sense.
It can provide you with tools for life
Cognitive behaviour therapy teaches strategies and equips you with tools to help you look after your own mental health. Tools like problem solving skills, once learned can be applied to a range of different situations.
It focusses more on the here and now
While a certain amount of history is required, the focus of CBT is on the present. CBT takes a problem-solving approach and focusses on developing skills to improve our current state of mind.
Supported by scientific research
Cognitive behaviour therapy is one of the most widely researched forms of therapy. There is a strong evidence base that CBT can improve the lives of people living with a range of mental and physical conditions. Furthermore, the effects of CBT can be long lasting (Hoffman, 2012).
Goal orientated and time based
Cognitive behaviour therapy is a structured and goal orientated form of therapy. It is time based. For example a goal for a patient with obsessive compulsive disorder may be to reduce the time spent washing hands from five hours per day to one hour per day by the end of week three of therapy (Harden, 2012). Overall, CBT can also take less time than other psychological therapy techniques to produce results.
CBT has a broad application
Cognitive behaviour therapy can treat a number of conditions either alone or in combination with other therapies. It can also support coping with several different life events. Some of the conditions that CBT can treat include:
Major depressive disorder
Bipolar disorder
Schizophrenia
Generalised anxiety disorder
Panic disorder
Obsessive compulsive disorder
Post traumatic disorder
Bulimia
Anorexia nervosa
Addiction
Stress management
Chronic pain
Phobias
Is Cognitive Behaviour Therapy For Me?
You may be wondering if cognitive behaviour therapy is for you? While cognitive behaviour therapy is an established treatment for a range of conditions there are a few things to be prepared for which include:
Being ready for self reflection
Cognitive behaviour therapy involves examining our thoughts and behaviours. It can also require us to challenge certain unhelpful assumptions and long held beliefs we may have that shape the way we see ourselves, others and the world. This requires a level of self reflection and open mindedness.
Motivation – Putting in the work
Like most things, cognitive behaviour therapy does require engagement and commitment to see best results. This includes attending therapy sessions and completing any homework or practical exercises. Part of the therapy process may be to complete certain tasks in between sessions. These tasks will help to reinforce cognitive and behavioural skills and strategies being learnt in session. In a sense, the tasks help you put the therapy into action in everyday life.
Tasks set will be specifically tailored to your personal therapy goals. Tasks can include things like:
1. Different types of writing exercises. For example, keeping a record evaluating and responding to unhelpful thoughts and behaviours.
2. Practising relaxation techniques
3. Behaviour activation – scheduling meaningful activities such as exercise, social outings or activities that bring enjoyment
4. Completing specific behavioural experiments that are set with your therapist. Behavioural experiments can be set to challenge a persons automatic thoughts and entrenched assumptions. For example, someone seeking therapy for social anxiety may set a task to attend a small social gathering.
Cognitive Behavioural Therapy Near Me
Studies have shown that cognitive behavioural therapy delivered by telehealth can be just as effective as in person. At Jelly Health we provide access to psychology services via telehealth (video) Australia wide. To schedule an appointment with one of our psychologists, submit and enquiry or call 1300 281 540
References
Beck J, Fleming S. A ( 2021) Brief History of Aaron T. Beck, MD, and Cognitive Behavior Therapy. Clin Psychol Eur. Jun 18;3(2):e6701.
Briers S. (2014). Brilliant Cognitive Behavioural Therapy. 2nd Edition. Pearson.
Chand S, Kuckel D, Huecker M. (2023). Cognitive Behaviour Therapy. StatPearls Publishing LLC
Fordham B, Sugavanam T, Edwards K, et al. (2021). The evidence for cognitive behavioural therapy in any condition, population or context: a meta-review of systematic reviews and panoramic meta-analysis. Psychological Medicine.51(1):21-29.
Fenn K, Byrne M. (2013). The key principles of cognitive behavioural therapy. InnovAiT. 6(9):579-585
Hofmann S, Asnaani A, Vonk I, Sawyer A, Fang A. 2012. The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognit Ther Res. Oct 1;36(5):427-440.
Harden M, (2012). Cognitive behaviour therapy. Incorporating therapy into general practice. Australian Family Physician, Vol 41. No 9. September 2012
What is cognitive behaviour therapy. 2017. Source: APA Div. 12 (Society of Clinical Psychology)